First injection to stop HIV approved

Michelle Robertsdigital health editor
 Getty Images
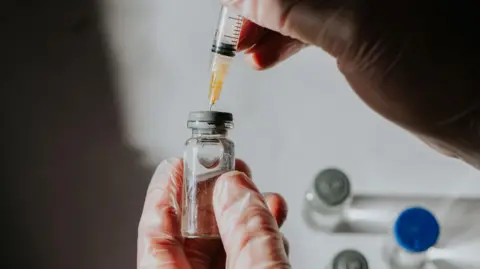
Getty ImagesAn HIV prevention injection will be offered to NHS patients for the first time in England and Wales, bringing the policy into line with Scotland.
The long-acting vaccine, given six times a year or every two months, is an alternative to taking a daily pill to protect against the virus.
Experts hope cabotegravir (CAB-LA) injections will help meet the target of ending new cases of HIV in the UK by 2030.
Meanwhile, early results from a different injection called lenacapavir suggest it might even be possible to switch people to another injection. annual HIV prevention vaccination.
‘This represents hope’
Secretary of State for Health and Social Care Wes Streeting said: “The approval of this game-changing injection perfectly embodies what this government is determined to deliver: cutting-edge treatments that save lives and leave no one behind.
“This represents hope for vulnerable people who cannot use other methods of preventing HIV.”
HIV prevention treatment, known as PrEP (pre-exposure prophylaxis), is taken by HIV-negative people to reduce their risk of contracting HIV.
The pills have been available for years and are still highly effective at stopping HIV infections, but they are not always easy for some to take.
It may be difficult to access, impractical, or embarrassing. For example, people may worry that someone, such as their parent or roommate, might find their pills.
Homelessness and domestic violence can make it difficult to take oral PrEP every day.
An injection that lasts for months offers convenience and confidentiality.
HIV is a virus that damages cells in the immune system and weakens the body’s ability to fight daily infections and diseases.
It can be caught during unprotected sexual intercourse or by sharing needles. Mothers can also infect their babies at birth.
Cabotegravir should be used in conjunction with safer sex practices such as condom use.
The NHS has an undisclosed discount from the manufacturer for the treatment, which has a list price of around £7,000 per patient per year.
The vaccine will be considered for healthy-weight adults and adolescents who are at high risk for sexually transmitted HIV and who are eligible for PrEP but for whom oral tablets would be difficult to obtain. It is thought that approximately 1000 people will be offered offers.
They’ll be able to get it from NHS-run sexual health clinics “in the coming months” National Institute for Health and Care Excellence (BEAUTIFUL).
Charities say some people are facing long waiting times for appointments at clinics and the rollout needs to happen quickly.
Richard Angell, of the Terrence Higgins Trust, said it was time to introduce “transformative therapy” not just in sexual health clinics but in other settings as well.
“It is highly effective and acceptable to patients, and is a vital tool in tackling inequalities, with the potential to reach people who are currently unable to access other methods of HIV prevention.”
official figures It shows that the number of people taking PrEP in sexual health services for England is increasing.
Last year, 146,098 HIV-negative people accessing sexual health services required PrEP because they were at significant risk of contracting HIV.
Of these, approximately 76% (111,123) started or continued PrEP; 7.7% increase compared to 2023.
However, the need for PrEP is not determined and met fairly.
Access to treatment varies significantly by group; This rate is highest among white (79.4%) and ethnic minority (77.8%) gay, bisexual and all men who have sex with men, but much lower among black African heterosexual women (34.6%) and men (36.4%).
At the same time, HIV testing has become widespread in hospital A&E departments in England. Currently, 89 people routinely test everyone who receives blood, especially in cities and towns where HIV prevalence is high.




